Exercise For Polycystic Ovarian Syndrome (PCOS)
What is PCOS?
PCOS is the most common hormonal disorder among women of reproductive age.
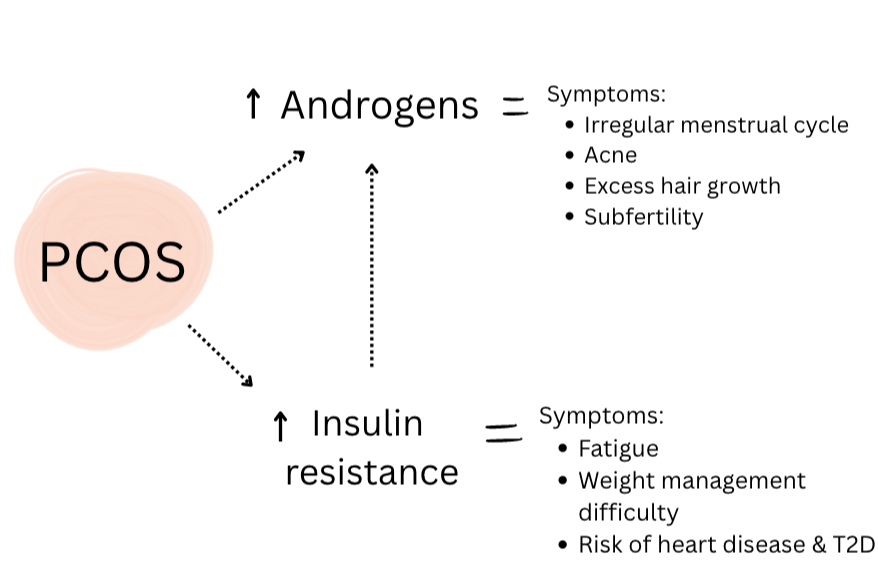
It’s quite a complex condition where we see a hormonal imbalance:
⬆️ higher than normal levels of a hormone called androgen leading to a spectrum of symptoms such as irregular menstrual cycles, unwanted hair growth, acne and subfertility.
⬆️ higher levels of insulin or insulin resistance which actually contribute to more androgen production which exacerbate symptoms.
Although common, the delay in diagnosis and uncertainty in management combined with the disheartening symptoms of PCOS can be quite frankly, frustrating for women.
It has a big impact on women’s mental health with 36% of women experiencing depression, 42% experiencing anxiety and over 70% of women report body image distress.
At Strength By Women, we are passionate about working with women diagnosed with PCOS because we know exercise can help mitigate the clinical features of PCOS and positively impact mental and physical health.
How is PCOS diagnosed?
The Rotterdam diagnostic criteria is used to diagnose PCOS, with women having at least two of the following:
1) Oligomenorrhea/anovulation
2) High levels of androgens (and other hormonal markers)
3) Polycystic ovaries (PCO)
There are 4 types categorised as:
Phenotype A: has all 3 of the above (accounting for 66%)
Phenotype B: Ovulatory PCOS (hyperandrogenism, PCO, regular menstrual cycles)
Phenotype C: Non-PCO PCOS (irregular menstrual cycle, hyperandrogenism, normal ovaries)
Phenotype D: Normoandrogenic PCOS (irregular menstrual cycles, PCO, normal androgen levels)
Due to the varying types, there is a large spectrum of symptoms that arise with PCOS and therefore, management strategies need to be individualised.
The Hormonal Imbalance: Androgens & Insulin
Androgens are not all bad.
They exist to convert into estrogen which supports follicular development and ovulation for a healthy menstrual cycle.
However, when made in excess, follicles don’t develop properly and ovulation is disrupted leading to irregular menstrual cycles.
Add to the mix, insulin resistance… women then enter into a vicious cycle because more insulin makes more androgen.
What is insulin resistance?
Put simply, insulin is the hormone responsible for managing blood sugar by allowing sugar to move into tissues, such as muscle, to be used as energy.
When the body doesn’t respond to insulin properly, it produces more and becomes de-sensitised to it.
This results in sugar build up in the blood where muscles can’t access it to use it for energy.
Some symptoms that arise are fatigue, weight gain (especially around the mid-section), increased risk of cardiovascular disease and type 2 diabetes and worsening of PCOS symptoms.
How Can Exercise Help Women With PCOS?
What the Research Suggests:
Exercises improves insulin function, and this:
a) Dampens excess androgen production
b) Gives muscles access to sugar from the blood for energy
The best exercise types for hormonal balance are HIIT, strength training and combined (strength & aerobic).
Note: When it comes to hormones such as androgens, testosterone, SHBG research suggests strength and combined training can improve these.Exercise can reduce fat (especially belly fat/visceral fat) and increase muscle which then increases metabolism (how much energy we burn at rest).
The best exercise types are HIIT and combined training.
Note: there needs to be more research looking into this with more accurate ways of measuring body composition…Exercise helps regulate menstrual cycles and fertility outcomes.
Any mode of exercise improves reproductive outcomes and the best exercise types are HIIT and combined training for menstrual cycle regularity.Exercise improves cardiovascular fitness:
Both high and moderate intensity aerobic exercise increase cardiovascular fitness (VO2max) however, HIIT is more potent.Exercise improves mental health: Any structured exercise appears beneficial, with moderate-to-vigorous intensity showing the greatest effects.
PCOS symptoms increase as body weight increases and therefore weight management is one of the most powerful ways to manage PCOS symptoms for women with a BMI >25.
It’s reported about 75% of lean women with PCOS are insulin resistant so even if weight loss may not be the focus for women with a BMI<25, exercise can significantly improve insulin function.
No wonder exercise is currently the first line of treatment for PCOS! It comes with additional health benefits while targeting a major root cause with no adverse side effects.
What the Research Tells Us (and Doesn’t)
Exercise recommendations for women with PCOS lacks specificity and are broad because more research is needed to determine exact training prescriptions for the type, intensity, frequency, and duration.
This means individualisation of an exercise program is even more important due to the complex and variable nature of the condition.
What we do know is exercise improves the hormonal and metabolic dysfunctions at the core of PCOS even before significant weight loss and this gives us a solid foundation to start from.
How We Tailor Exercise for Women With PCOS
Our clinic specialises in helping women ease into these evidence-based protocols safely and confidently.
We start where you are:
If you haven’t exercised in a while, or you’re unsure how you can fit exercise into your schedule, it’s okay. Your program begins at a level that feels doable, even if it’s once a fortnight, and we build from there.
We customise it to you:
Strength, moderate intensity aerobic, high intensity aerobic, combination? We create a plan suitable to you while still working towards evidence-based protocols.
We keep it sustainable:
We’re always thinking long term so we work with you to find the right balance between dose and rest so your body can adapt, not burn out.
We work with your GP:
Exercise doesn’t replace medical advice so we work closely with your healthcare team to ensure your exercise plan fits your overall management strategy.
If you have recently been diagnosed or have been living with PCOS symptoms and feeling a little lost or overwhelmed, please reach out as we’d love to meet you and discuss how we can help you feel at home in your body again.
Every success story in our clinic began with the first step of trying exercise as medicine.
References
Stepto, N. K., Cassar, S., Joham, A. E., Hutchison, S. K., Harrison, C. L., Goldstein, R. F., & Teede, H. J. (2013). Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Human reproduction (Oxford, England), 28(3), 777–784.
Patten, R. K., Pascoe, M. C., Moreno-Asso, A., Boyle, R. A., Stepto, N. K., & Parker, A. G. (2021). Effectiveness of exercise interventions on mental health and health-related quality of life in women with polycystic ovary syndrome: A systematic review. BMC Public Health, 21, 2310.
Patten, R. K., McIlvenna, L. C., Levinger, I., Garnham, A. P., Shorakae, S., Parker, A. G., … & Stepto, N. K. (2022). High-intensity training elicits greater improvements in cardio-metabolic and reproductive outcomes than moderate-intensity training in women with PCOS: A randomized clinical trial. Human Reproduction, 37(5), 1018–1029.
Teede, H. J., Joham, A. E., Paul, E., Moran, L. J., Loxton, D., Jolley, D., & Lombard, C. (2013). Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obesity (Silver Spring, Md.), 21(8), 1526–1532.
Lucidi, R. S. (2023). Polycystic Ovarian Syndrome: Treatment & Management. Medscape. Retrieved July 23, 2025, from https://emedicine.medscape.com/article/256806-treatment
Almenning, I., Rieber-Mohn, A., Lundgren, K. M., Shetelig Løvvik, T., Garnæs, K. K., & Moholdt, T. (2015). Effects of High Intensity Interval Training and Strength Training on Metabolic, Cardiovascular and Hormonal Outcomes in Women with Polycystic Ovary Syndrome: A Pilot Study. PloS one, 10(9), e0138793.
Nasiri, M., Monazzami, A., Alavimilani, S., & Asemi, Z. (2025). Modulation of hormonal, metabolic, inflammatory and oxidative stress biomarkers in women with polycystic ovary syndrome following combined (resistant and endurance) training: A randomized controlled trial. BMC Endocrine Disorders, 25, Article 1.
Harrison, C. L., Lombard, C. B., Moran, L. J., & Teede, H. J. (2011). Exercise therapy in polycystic ovary syndrome: a systematic review. Human reproduction update, 17(2), 171–183.
Butt, M. S., Saleem, J., Zakar, R., Aiman, S., Khan, M. Z., & Fischer, F. (2023). Benefits of physical activity on reproductive health functions among polycystic ovarian syndrome women: a systematic review. BMC public health, 23(1), 882.
Vizza, L., Smith, C. A., Swaraj, S., Agho, K., & Cheema, B. S. (2016). The feasibility of progressive resistance training in women with polycystic ovary syndrome: A pilot randomized controlled trial. BMC Sports Science, Medicine and Rehabilitation, 8, Article 14.
Bozdag, G., Mumusoglu, S., Zengin, D., Karabulut, E. & Yildiz, B. O. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod 31, 2841-2855,
Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertility and Sterility, Volume 81, Issue 1, 19 - 25
Cooney, L. G., Lee, I., Sammel, M. D., & Dokras, A. (2017). High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Human reproduction (Oxford, England), 32(5), 1075–1091.